Osteoarthritis: Difference between revisions
| (28 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
==Background== | ==Background== | ||
*Osteoarthritis is a chronic arthropathy characterized by degeneration of joint cartilage and underlying bone | |||
*Alternatively called arthrosis<ref>KELLGREN JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502. doi:10.1136/ard.16.4.494</ref> | |||
*Most common progressive joint disease | |||
*Joints in the hands, knees, hips, and spine are the most frequently affected. | |||
===Risk Factors=== | |||
*Age (almost exclusively in elderly) | |||
*Female versus male sex | |||
*Obesity | |||
*Lack of osteoporosis | |||
*Occupation | |||
*Previous injury | |||
*Muscle weakness | |||
*Genetic elements | |||
==Clinical Features== | ==Clinical Features== | ||
[[File:Osteoarthritis.jpg|thumb|PIP (Bouchard's nodes) and DIP (Heberden's node) inflamation.]] | |||
[[File:Areas affected by osteoarthritis.gif|thumb|Most commonly affected joints.]] | |||
*Commonly affected joints | *Commonly affected joints | ||
**Cervical and lumbar spine | **Cervical and lumbar spine | ||
| Line 27: | Line 34: | ||
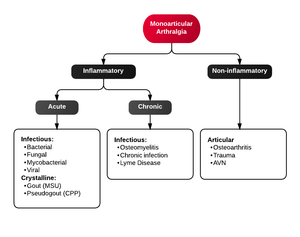
==Differential Diagnosis== | ==Differential Diagnosis== | ||
{{Differential Diagnosis Monoarthritis}} | |||
{{Differential Diagnosis Polyarthritis}} | {{Differential Diagnosis Polyarthritis}} | ||
== | ==Evaluation== | ||
[[File:Osteoarthritis left knee.jpg|thumb|OA of left knee]] | |||
[[File:Osteo of the hand.jpg|thumb|OA and osteopenia of the carpal joint and 1st carpometacarpel joint]] | |||
*Greater than 50 years of age | *Greater than 50 years of age | ||
*Morning stiffness for less than 30 minutes | *Morning stiffness for less than 30 minutes | ||
| Line 41: | Line 49: | ||
==Management== | ==Management== | ||
===Nonpharmacological=== | |||
*Weight loss | |||
*Ice/warm packs | |||
*Physical therapy | |||
*Occupational therapy | |||
*Exercise | |||
===Pharmacological <ref> Jordan JM, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007 Jan. 34(1):172-80. </ref>=== | |||
*Topical [[capsaicin]] | |||
*Topical [[NSAIDs]] | |||
*Oral [[NSAIDs]] | |||
*[[Tylenol]] | |||
*Steroid injections | |||
*[[Tramadol]] | |||
===AAOS Decision Tool for Knee OA=== | |||
*Refer to this helpful tool from the American Academy of Orthopedic Surgeons for management and disposition options | |||
*[http://www.orthoguidelines.org/go/auc/auc.cfm?auc_id=224986 Link to knee osteoarthritis tool] | |||
===Surgical=== | |||
*Arthroscopy for removal of meniscal tears or loose foreign bodies | |||
**No additional benefit compared to PT and medical therapy in routine OA <ref> Kirkley A, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008 Sep 11. 359(11):1097-107 </ref> | |||
*Osteotomy in young patients with misalignment of knee or hip joint | |||
*Arthroplasty | |||
**If all other modalities are ineffective | |||
**Prothetic knee/hip/shoulder usually has 10-15 year viability | |||
**Infection, [[Pulmonary embolism]] are biggest risks | |||
*Joint fusion | |||
**Relieves pain but prevents motion | |||
**May be used in small foot/ankle bones or after failed arthroplasties | |||
==Disposition== | ==Disposition== | ||
*Discharge with PCP follow-up | |||
==See Also== | ==See Also== | ||
*[[Arthritis]] | |||
==External Links== | ==External Links== | ||
*[https://www.merckmanuals.com/professional/musculoskeletal-and-connective-tissue-disorders/joint-disorders/osteoarthritis-oa Merck Manual - Osteoarthritis (OA)] | |||
==References== | ==References== | ||
<references/> | |||
[[Category:Orthopedics]] | |||
Latest revision as of 13:27, 19 September 2021
Background
- Osteoarthritis is a chronic arthropathy characterized by degeneration of joint cartilage and underlying bone
- Alternatively called arthrosis[1]
- Most common progressive joint disease
- Joints in the hands, knees, hips, and spine are the most frequently affected.
Risk Factors
- Age (almost exclusively in elderly)
- Female versus male sex
- Obesity
- Lack of osteoporosis
- Occupation
- Previous injury
- Muscle weakness
- Genetic elements
Clinical Features
- Commonly affected joints
- Cervical and lumbar spine
- First carpometacarpal joint
- Proximal interphalangeal joint
- Distal interphalangeal joint
- Hip
- Knee
- Subtalar joint
- First metatarsophalangeal joint
- Uncommonly affected joints
- Shoulder
- Wrist
- Elbow
- Metacarpophalangeal joint
Differential Diagnosis
Monoarticular arthritis
- Acute osteoarthritis
- Avascular necrosis
- Crystal-induced (Gout, Pseudogout)
- Gonococcal arthritis, arthritis-dermatitis syndrome
- Nongonococcal septic arthritis
- Lyme disease
- Malignancy (metastases, osteochondroma, osteoid osteoma)
- Reactive poststreptococcal arthritis
- Trauma-induced arthritis
- Fracture
- Ligamentous injury
- Overuse
- Avascular necrosis
- Decompression sickness
- Spontaneous osteonecrosis
- Hemorrhagic (e.g. hemophilia, systemic anticoagulation
- Seronegative spondyloarthropathies (ankylosing spondylitis, IBD, psoriatic arthritis, reactive arthritis
- RA, SLE
- Sarcoidosis, amyloidosis
- Periarticular pathology
- Transient (Toxic) Synovitis (Hip)
- Slipped Capital Femoral Epiphysis (SCFE)
- Legg Calve Perthes Disease
Polyarthritis
- Fibromyalgia
- Juvenile idiopathic arthritis
- Lyme disease
- Osteoarthritis
- Psoriatic arthritis
- Reactive poststreptococcal arthritis
- Rheumatoid arthritis
- Rheumatic fever
- Serum sickness
- Systemic lupus erythematosus
- Serum sickness–like reactions
- Viral arthritis
Evaluation
- Greater than 50 years of age
- Morning stiffness for less than 30 minutes
- Crepitus on active motion of the knee
- Bony tenderness
- Bony enlargement
- No palpable warmth
Management
Nonpharmacological
- Weight loss
- Ice/warm packs
- Physical therapy
- Occupational therapy
- Exercise
Pharmacological [2]
AAOS Decision Tool for Knee OA
- Refer to this helpful tool from the American Academy of Orthopedic Surgeons for management and disposition options
- Link to knee osteoarthritis tool
Surgical
- Arthroscopy for removal of meniscal tears or loose foreign bodies
- No additional benefit compared to PT and medical therapy in routine OA [3]
- Osteotomy in young patients with misalignment of knee or hip joint
- Arthroplasty
- If all other modalities are ineffective
- Prothetic knee/hip/shoulder usually has 10-15 year viability
- Infection, Pulmonary embolism are biggest risks
- Joint fusion
- Relieves pain but prevents motion
- May be used in small foot/ankle bones or after failed arthroplasties
Disposition
- Discharge with PCP follow-up
See Also
External Links
References
- ↑ KELLGREN JH, LAWRENCE JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502. doi:10.1136/ard.16.4.494
- ↑ Jordan JM, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007 Jan. 34(1):172-80.
- ↑ Kirkley A, et al. A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2008 Sep 11. 359(11):1097-107