Narrow-complex tachycardia: Difference between revisions
m (Rossdonaldson1 moved page Narrow complex tachycardia to Narrow-complex tachycardia) |
|||
| (28 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
*Heart rate > 100 bpm | *Heart rate > 100 bpm | ||
*Originates above the ventricles | *Originates above the ventricles | ||
==Clinical Features== | ==Clinical Features== | ||
*Heart rate > 100 bpm | *Heart rate > 100 bpm | ||
*May have: | *May have: | ||
**Palpitations | **[[Palpitations]] | ||
**Syncope or pre-syncope | **[[Syncope]] or pre-syncope | ||
**Chest pain | **[[Chest pain]] | ||
**Dyspnea | **[[Dyspnea]] | ||
**Altered level of consciousness | **[[Altered level of consciousness]] | ||
**Delayed capillary refill | **Delayed capillary refill | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
{{Tachycardia (narrow) DDX}} | |||
{{Tachycardia (wide) DDX}} | |||
==Evaluation== | ==Evaluation== | ||
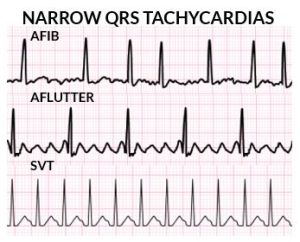
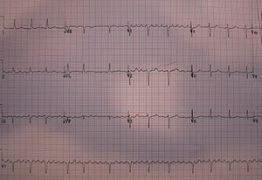
[[File:Narrow Complex Atrial Tachycardias.jpg|thumb|Examples of '''narrow'''-complex tachycardias.]] | |||
===Workup=== | |||
*[[ECG]] | |||
===Diagnosis=== | |||
*Flutter vs coarse AFib: determine atrial regularity by taking big bites | |||
===Narrow-complex tachycardia comparison table=== | |||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 88: | Line 79: | ||
|} | |} | ||
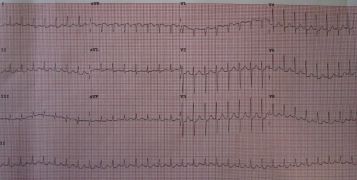
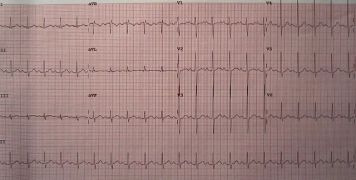
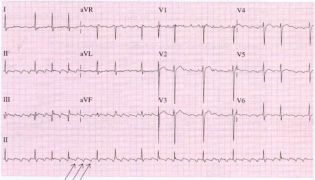
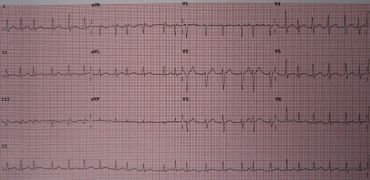
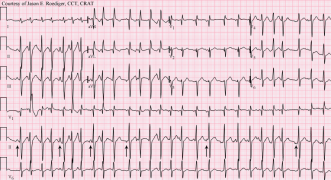
===Narrow-Complex Tachycardia Examples=== | |||
<gallery mode="packed"> | |||
File:SVT12.jpg|[[PSVT]] | |||
File:Sinustachy.jpg|[[Sinus tachycardia]]]] | |||
File:Aflutter.jpg|[[Atrial flutter]] (with alternating 2:1 and 3:1 block). | |||
File:Atrial flutter.jpg|[[Atrial flutter]] (with variable block) | |||
File:PAC.png|[[PACs]] | |||
File:Afib.jpg|[[Atrial fibrillation]] | |||
File:Multifocal atrial tachycardia - MAT.png|[[Multifocal atrial tachycardia]] | |||
</gallery> | |||
==Management== | ==Management== | ||
| Line 99: | Line 99: | ||
*Cardioversion: [[Sotalol]], [[cardioversion|electric]] | *Cardioversion: [[Sotalol]], [[cardioversion|electric]] | ||
===Junctional=== | ===[[Junctional tachycardia]]=== | ||
*Treat underlying cause | *Treat underlying cause | ||
*Consider: | *Consider: | ||
**Amiodarone | **[[Amiodarone]] | ||
**Beta-blocker | **[[Beta-blocker]] | ||
**Calcium-channel blocker | **[[Calcium-channel blocker]] | ||
==Disposition== | ==Disposition== | ||
| Line 112: | Line 112: | ||
==See Also== | ==See Also== | ||
*[[Tachycardia]] | |||
*[[ACLS: Tachycardia]] | *[[ACLS: Tachycardia]] | ||
*[[V Tach vs. SVT]] | *[[V Tach vs. SVT]] | ||
| Line 118: | Line 119: | ||
==External Links== | ==External Links== | ||
==References== | ==References== | ||
Latest revision as of 17:21, 30 July 2025
Background
- Heart rate > 100 bpm
- Originates above the ventricles
Clinical Features
- Heart rate > 100 bpm
- May have:
- Palpitations
- Syncope or pre-syncope
- Chest pain
- Dyspnea
- Altered level of consciousness
- Delayed capillary refill
Differential Diagnosis
Narrow-complex tachycardia
- Regular
- AV Node Independent
- Sinus tachycardia
- Atrial tachycardia (uni-focal or multi-focal)
- Atrial fibrillation
- Atrial flutter
- Idiopathic fascicular left ventricular tachycardia
- AV Node Dependent
- AV Node Independent
- Irregular
- Multifocal atrial tachycardia (MAT)
- Sinus tachycardia with frequent PACs, PJCs, PVCs
- Atrial fibrillation
- Atrial flutter with variable conduction
- Digoxin Toxicity
Wide-complex tachycardia
Assume any wide-complex tachycardia is ventricular tachycardia until proven otherwise (it is safer to incorrectly assume a ventricular dysrhythmia than supraventricular tachycardia with abberancy)
- Regular
- Monomorphic ventricular tachycardia
- PSVT with aberrant conduction:
- PSVT with bundle branch block^
- PSVT with accessory pathway
- Atrial flutter with bundle branch block^
- Sinus tachycardia with bundle branch block^
- Accelerated idioventricular rhythm (consider if less than or ~120 bpm)
- Metabolic
- Irregular
- Atrial fibrillation/atrial flutter with variable AV conduction AND bundle branch block^
- Atrial fibrillation/atrial flutter with variable AV conduction AND accessory pathway (e.g. WPW)
- Atrial fibrillation + hyperkalemia
- Polymorphic ventricular tachycardia
^Fixed or rate-related
Evaluation
Workup
Diagnosis
- Flutter vs coarse AFib: determine atrial regularity by taking big bites
Narrow-complex tachycardia comparison table
| Differential | A.Rhythm | A.rate | A.morphology | Vagal/adenosine |
| A fib | Irregular | >350 | Fibrillatory (V1) | Incr. AV block |
| A Flutter | Regular | >250, <350 | Sawtooth (II, III, AVF) | Incr. AV block |
| A Tach | Regular | >100 | Neg in II, III, AVF | Nothing |
| AVNRT (SVT) | Regular | >160 | No p's | → NSR |
| Junctional | Regular | >100, <150 | No p's or retrograde p's | Nothing |
| MAT | Irregular | >100 | >3 distinct p shapes | Transient slowing |
| Sinus tachycardia | Regular |
>100 <180 |
Normal | Transient slowing |
Narrow-Complex Tachycardia Examples
Atrial flutter (with alternating 2:1 and 3:1 block).
Atrial flutter (with variable block)
Management
<translate>
Narrow Regular Tachycardia
- Sinus tachycardia
- Treat underlying cause
- SVT
- Vagal maneuvers (convert up to 25%)
- Adenosine 6mg rapid IV push if patient hemodynamically stable (unstable should proceed directly to electrical cardioversion)
- Can follow with repeat dose of 6 mg or 12mg if initially fails
- If adenosine fails, initiate rate control with calcium channel blocker or beta blocker or use synchronized cardioversion
- Diltiazem 15-20mg IV, followed by infusion of 5-15mg/hr
- Metoprolol 5mg IVP x 3 followed by 50mg PO
- Synchronized cardioversion (50-100J)
- Provide sedation prior to synchronized cardioversion if patient is hemodynamically stable
- Atrial flutter
- Stable: Consider rate control to HR < 110 bpm
- Unstable: Synchronized cardioversion; start at 50J
</translate>
<translate>
Narrow Irregular Tachycardia
- Multi-focal atrial tachycardia (MAT)
- Treat underlying cause (hypokalemia, hypomagnesemia)
- Consider diltiazem
- Avoid beta blockers unless they are already known to be tolerated, as airway disease often co-morbid
- If not symptomatic and rate < 110/120 bpm, may not require treatment (e.g., patient with MAT secondary to COPD)
- Sinus tachycardia with frequent PACs
- Treat underlying cause
- A fib / A Flutter with variable conduction (see also Atrial Fibrillation with RVR)
- Check if patient has taken usual rate-control meds
- If missed dose, may provide dose of home medication and observe for resolution
- Determine whether patient is better candidate for rate control or rhythm control [1]
- Rate control preferred with:
- Persistent A fib
- Less symptomatic patients
- Age 65 or older
- Hypertension
- No heart failure
- Previous failure to cardiovert
- Patient preference
- Rhythm control preferred with:
- Rate control preferred with:
- Rate control with:
- Diltiazem
- Metoprolol
- Amiodarone (good in setting of hypotension, CHF)
- Digoxin (good in setting of CHF)
- Rhythm conversion with:
- Synchronized Cardioversion (120-200 J)
- Best performed on patients with new onset A fib or patients fully therapeutically anti-coagulated for > 3 weeks
- Procainamide per Ottawa Aggressive ED Cardioversion Protocol
- Synchronized Cardioversion (120-200 J)
- Check if patient has taken usual rate-control meds
</translate>
Atrial fibrillation with RVR/flutter
- Rate control: Diltiazem, metoprolol, digoxin
- Dig usually only helpful when already with a block (e.g. 2:1)
- Cardioversion: Sotalol, electric
Junctional tachycardia
- Treat underlying cause
- Consider:
Disposition
- Stable patients without serious comorbid illness who are adequately rate or rhythm controlled can be discharged home with follow-up
- Patients with acute underlying cause may require admission
- Patients who cannot achieve asymptomatic rate or rhythm control may require admission
See Also
External Links
References
- ↑ Frankel, G. et al. (2013) Rate versus rhythm control in atrial fibrillation. Canadian Family Physician 59(2), 161 - 168