Ischemic colitis: Difference between revisions
Ostermayer (talk | contribs) (Prepared the page for translation) |
|||
| (10 intermediate revisions by one other user not shown) | |||
| Line 1: | Line 1: | ||
<languages/> | |||
<translate> | |||
==Background== | ==Background== | ||
[[File:Diameters of the large intestine.png|thumb|Average inner diameters and ranges of different sections of the large intestine.<ref> Nguyen H, Loustaunau C, Facista A, Ramsey L, Hassounah N, Taylor H, et al. (July 2010). "Deficient Pms2, ERCC1, Ku86, CcOI in field defects during progression to colon cancer". Journal of Visualized Experiments (41). doi:10.3791/1931. PMC 3149991. PMID 20689513.</ref>]] | |||
</translate> | |||
{{Intestinal ischemia types}} | {{Intestinal ischemia types}} | ||
<translate> | |||
===Risk Factors=== | ===Risk Factors=== | ||
*[[Constipation]] (increased intraluminal pressure compresses vessels) | |||
*[[IBS]] | *[[Special:MyLanguage/Constipation|Constipation]] (increased intraluminal pressure compresses vessels) | ||
*[[Special:MyLanguage/IBS|IBS]] | |||
*Vascular risk factors | *Vascular risk factors | ||
*[[COPD]] (risk doubles)<ref>Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg. 2012 Dec;25(4):228-35. doi: 10.1055/s-0032-1329534. PMID: 24294125; PMCID: PMC3577613.</ref> | *[[Special:MyLanguage/COPD|COPD]] (risk doubles)<ref>Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg. 2012 Dec;25(4):228-35. doi: 10.1055/s-0032-1329534. PMID: 24294125; PMCID: PMC3577613.</ref> | ||
*Females > Males | *Females > Males | ||
==Clinical Features== | ==Clinical Features== | ||
*Consider | |||
* | ''*Consider in all patients patients ≥50 years old with acute-onset abdominal pain and cardiovascular morbidities.<ref>[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net]</ref>'' | ||
* Typically presents with: | |||
* | **[[Special:MyLanguage/Bloody diarrhea|Bloody diarrhea]] | ||
* | **Diffuse [[Special:MyLanguage/abdominal pain|abdominal pain]] | ||
* | |||
* | |||
* | ===Precipitants=== | ||
* | |||
* | ''Can be precipitated by any illness that decreases flow to the colon.'' | ||
** Cocaine | *[[Special:MyLanguage/Hypovolemia|Hypovolemia]] | ||
** Anti- | *[[Special:MyLanguage/Blood loss|Blood loss]] | ||
** Diuretics | *[[Special:MyLanguage/Dialysis|Dialysis]] | ||
** Digitalis | *[[Special:MyLanguage/Anaphylaxis|Anaphylaxis]] | ||
** Carboplatin- | *[[Special:MyLanguage/Pancreatitis|Pancreatitis]] | ||
** Vasopressors | *[[Special:MyLanguage/Drugs|Drugs]]: | ||
** Pseudoephedrine | * [[Special:MyLanguage/NSAIDs|NSAIDs]] | ||
** [[Special:MyLanguage/Cocaine|Cocaine]] | |||
** [[Special:MyLanguage/Anti-hypertensives|Anti-hypertensives]] | |||
** [[Special:MyLanguage/Diuretics|Diuretics]] | |||
** [[Special:MyLanguage/Digitalis|Digitalis]] | |||
** Carboplatin-paclitaxel | |||
** [[Special:MyLanguage/Vasopressors|Vasopressors]] | |||
** [[Special:MyLanguage/Pseudoephedrine|Pseudoephedrine]] | |||
** Triptans | ** Triptans | ||
** Interferon-Ribavirin | ** Interferon-[[Special:MyLanguage/Ribavirin|Ribavirin]] | ||
==Differential Diagnosis== | ==Differential Diagnosis== | ||
</translate> | |||
{{Colitis types}} | {{Colitis types}} | ||
<translate> | |||
</translate> | |||
{{Abdominal Pain DDX Diffuse}} | {{Abdominal Pain DDX Diffuse}} | ||
<translate> | |||
==Evaluation== | ==Evaluation== | ||
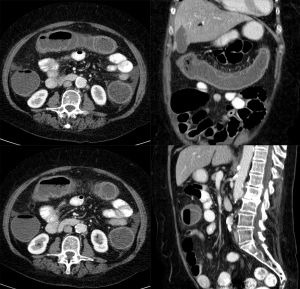
[[File:Ischaemische Colitis 67W - CT - 001.jpg|thumb|Ischemic colitis primarily in the transverse colon, confirmed endoscopically.]] | |||
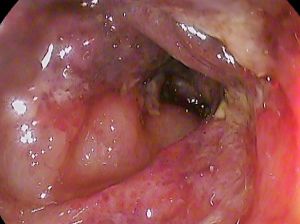
[[File:Ischemic colitis t-colon.jpg|thumb|Ischemic colitis of the transverse colon on endoscopy.]] | |||
===Workup=== | ===Workup=== | ||
* CBC to evaluate for quantity of blood loss | * CBC to evaluate for quantity of blood loss | ||
* CMP to evaluate for acute renal injury | * CMP to evaluate for acute renal injury | ||
* CT Abdomen and Pelvis with Contrast to evaluate for intestinal inflammation. | * CT Abdomen and Pelvis with Contrast to evaluate for intestinal inflammation. | ||
* May consider CTA to rule out mesenteric ischemia, but will rarely show large vessel occlusion. | * May consider CTA to rule out mesenteric ischemia, but will rarely show large vessel occlusion. | ||
===Diagnosis=== | ===Diagnosis=== | ||
* CT | |||
*Diagnosis is typically determined on abdominopelvic CT | |||
** Ischemic colitis most likely when found in splenic flexure or sigmoid colon. Ischemic colitis unlikely for colitis that localizes to other areas | |||
==Management== | ==Management== | ||
*Antibiotics, if the patient has any of the factors associated with severe disease.<ref>[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net]</ref> | |||
*[[Special:MyLanguage/Antibiotics|Antibiotics]], if the patient has any of the factors associated with severe disease.<ref>[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net]</ref> | |||
*Emergent surgical consultation for:<ref>[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net]</ref> | *Emergent surgical consultation for:<ref>[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net]</ref> | ||
**Peritoneal signs | **Peritoneal signs | ||
| Line 53: | Line 87: | ||
**Isolated right-colon ischemia on imaging | **Isolated right-colon ischemia on imaging | ||
* Improved hydration | * Improved hydration | ||
* Avoid NSAIDs | * Avoid [[Special:MyLanguage/NSAIDs|NSAIDs]] | ||
* Bowel rest with clear liquid diet | * Bowel rest with clear liquid diet | ||
==Disposition== | ==Disposition== | ||
* Admit patient with more severe symptoms. Pain uncontrolled, large volume blood loss, unable to tolerate PO. | |||
* Admit patient with more severe symptoms. Pain uncontrolled, large volume blood loss, unable to tolerate PO.<ref>Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg. 2012 Dec;25(4):228-35. doi: 10.1055/s-0032-1329534. PMID: 24294125; PMCID: PMC3577613.</ref> | |||
* Most patients can be discharged | * Most patients can be discharged | ||
* Need follow up colonoscopy in months to ensure no underlying etiology. | * Need follow up colonoscopy in months to ensure no underlying etiology. | ||
* Ensure future workup for younger patients | * Ensure future workup for younger patients | ||
**More likely to have underlying vasculitis or other cause. | **More likely to have underlying vasculitis or other cause. | ||
==See Also== | ==See Also== | ||
*[[Colitis]] | |||
*[[Mesenteric ischemia]] | *[[Special:MyLanguage/Colitis|Colitis]] | ||
*[[Special:MyLanguage/Mesenteric ischemia|Mesenteric ischemia]] | |||
==External Links== | ==External Links== | ||
*[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net] | *[http://www.emdocs.net/ischemic-colitis-ed-presentations-evaluation-and-management/ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net] | ||
==References== | ==References== | ||
<references/> | <references/> | ||
[[Category:GI]] | [[Category:GI]] | ||
[[Category:Surgery]] | [[Category:Surgery]] | ||
</translate> | |||
Latest revision as of 23:14, 4 January 2026
Background

Average inner diameters and ranges of different sections of the large intestine.[1]
Intestinal Ischemic Disorder Types
- Ischemic colitis
- Accounts for 80-85% of intestinal ischemia
- Due to non-occlusive disease with decreased blood flow to the colon.
- Causes decreased perfusion leading to sub-mucosal or mucosal ischemia only.
- Typical to the "watershed areas" of the colon (Splenic flexure or Sigmoid)
- Acute mesenteric ischemia
- Due to complete occlusion of mesenteric vessels
- Complete transmural ischemia
- Mesenteric venous thrombosis
- Chronic mesenteric ischemia ("intestinal angina")
Risk Factors
- Constipation (increased intraluminal pressure compresses vessels)
- IBS
- Vascular risk factors
- COPD (risk doubles)[2]
- Females > Males
Clinical Features
*Consider in all patients patients ≥50 years old with acute-onset abdominal pain and cardiovascular morbidities.[3]
- Typically presents with:
- Bloody diarrhea
- Diffuse abdominal pain
Precipitants
Can be precipitated by any illness that decreases flow to the colon.
- Hypovolemia
- Blood loss
- Dialysis
- Anaphylaxis
- Pancreatitis
- Drugs:
- NSAIDs
- Cocaine
- Anti-hypertensives
- Diuretics
- Digitalis
- Carboplatin-paclitaxel
- Vasopressors
- Pseudoephedrine
- Triptans
- Interferon-Ribavirin
Differential Diagnosis
Colitis
- Infectious colitis
- Ischemic colitis
- Ulcerative colitis
- CMV colitis
- Crohn's colitis
- Toxic colitis (antineoplastic agents)
- Pseudomembranous colitis
- Fibrosing colonopathy (Cystic fibrosis)
Diffuse Abdominal pain
- Abdominal aortic aneurysm
- Acute gastroenteritis
- Aortoenteric fisulta
- Appendicitis (early)
- Bowel obstruction
- Bowel perforation
- Diabetic ketoacidosis
- Gastroparesis
- Hernia
- Hypercalcemia
- Inflammatory bowel disease
- Mesenteric ischemia
- Pancreatitis
- Peritonitis
- Sickle cell crisis
- Spontaneous bacterial peritonitis
- Volvulus
Evaluation
Workup
- CBC to evaluate for quantity of blood loss
- CMP to evaluate for acute renal injury
- CT Abdomen and Pelvis with Contrast to evaluate for intestinal inflammation.
- May consider CTA to rule out mesenteric ischemia, but will rarely show large vessel occlusion.
Diagnosis
- Diagnosis is typically determined on abdominopelvic CT
- Ischemic colitis most likely when found in splenic flexure or sigmoid colon. Ischemic colitis unlikely for colitis that localizes to other areas
Management
- Antibiotics, if the patient has any of the factors associated with severe disease.[4]
- Emergent surgical consultation for:[5]
- Peritoneal signs
- Pneumatosis coli
- Portal venous gas
- Pan-colonic distribution, or
- Isolated right-colon ischemia on imaging
- Improved hydration
- Avoid NSAIDs
- Bowel rest with clear liquid diet
Disposition
- Admit patient with more severe symptoms. Pain uncontrolled, large volume blood loss, unable to tolerate PO.[6]
- Most patients can be discharged
- Need follow up colonoscopy in months to ensure no underlying etiology.
- Ensure future workup for younger patients
- More likely to have underlying vasculitis or other cause.
See Also
External Links
References
- ↑ Nguyen H, Loustaunau C, Facista A, Ramsey L, Hassounah N, Taylor H, et al. (July 2010). "Deficient Pms2, ERCC1, Ku86, CcOI in field defects during progression to colon cancer". Journal of Visualized Experiments (41). doi:10.3791/1931. PMC 3149991. PMID 20689513.
- ↑ Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg. 2012 Dec;25(4):228-35. doi: 10.1055/s-0032-1329534. PMID: 24294125; PMCID: PMC3577613.
- ↑ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net
- ↑ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net
- ↑ Shannon Thompson. Ischemic Colitis: ED Presentations, Evaluation, and Management emDOCs.net
- ↑ Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg. 2012 Dec;25(4):228-35. doi: 10.1055/s-0032-1329534. PMID: 24294125; PMCID: PMC3577613.