ACLS: Tachycardia: Difference between revisions
No edit summary |
|||
| Line 6: | Line 6: | ||
==[[Narrow complex tachycardia|'''Narrow''' complex tachycardia]]== | ==[[Narrow complex tachycardia|'''Narrow''' complex tachycardia]]== | ||
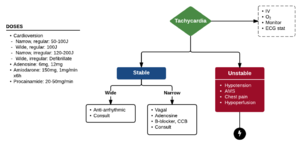
[[File:ACLS-tachycardia.png|thumb|Algorithm for tachycardia with a pulse (Adapted from ACLS 2010)]] | [[File:ACLS-tachycardia.png|thumb|Algorithm for tachycardia with a pulse (Adapted from ACLS 2010)]] | ||
{{ACLS Narrow Regular Tachycardia}} | |||
===[[ACLS]]: Narrow ''Irregular'' Tachycardia=== | ===[[ACLS]]: Narrow ''Irregular'' Tachycardia=== | ||
Revision as of 10:13, 14 March 2018
3 questions
- Is the patient in a sinus rhythm?
- Is the QRS wide or narrow?
- Is the rhythm regular or irregular?
Narrow complex tachycardia
Narrow Regular Tachycardia
- Sinus tachycardia
- Treat underlying cause
- SVT
- Vagal maneuvers (convert up to 25%)
- Adenosine 6mg rapid IV push if patient hemodynamically stable (unstable should proceed directly to electrical cardioversion)
- Can follow with repeat dose of 6 mg or 12mg if initially fails
- If adenosine fails, initiate rate control with calcium channel blocker or beta blocker or use synchronized cardioversion
- Diltiazem 15-20mg IV, followed by infusion of 5-15mg/hr
- Metoprolol 5mg IVP x 3 followed by 50mg PO
- Synchronized cardioversion (50-100J)
- Provide sedation prior to synchronized cardioversion if patient is hemodynamically stable
- Atrial flutter
- Stable: Consider rate control to HR < 110 bpm
- Unstable: Synchronized cardioversion; start at 50J
ACLS: Narrow Irregular Tachycardia
- MAT
- Treat underlying cause (hypoK, hypomag)
- Sinus Tachycardia with frequent PACs
- A fib / A Flutter with variable conduction (see also Atrial Fibrillation with RVR)
- Rate control with:
- Diltiazem
- MTP (good in setting of ACS)
- Amiodarone (good in setting of hypotension, CHF)
- Digoxin (good in setting of CHF)
- Synchronized Cardioversion (120-200 J)
- Rate control with:
Wide complex tachycardia
ACLS: Wide Regular Tachycardia
- If pulseless: shock (unsynchronized 200J)
- If unstable: shock (synchronized 100J)
- Hypotension, altered mental status, shock, ischemic chest discomfort, acute heart failure
- If stable:
- Meds
- Procainamide
- 20-50mg/min; then maintenance infusion of 1-4mg/min x6hr
- Treat until arrhythmia suppressed, QRS duration increases >50%, hypotension, Max 17mg/kg or 1 gram
- Avoid if prolonged QT or CHF
- Amiodarone
- 150mg over 10min (repeat as needed); then maintenance infusion of 1mg/min x6hr
- Adenosine
- May be considered for diagnosis and treatment only if rhythm is regular and monomorphic
- Procainamide
- Synchronized Cardioversion (100J)
- Meds
ACLS: Wide Irregular Tachycardia
DO NOT use AV nodal blockers as they can precipitate V-Fib
- A fib with preexcitation
- 1st line - Electric Cardioversion
- 2nd line - Procainamide, amiodarone, or sotalol
- A fib with aberrancy
- Polymorphic V-Tach / Torsades De Pointes
- Give IV MgSO4
- Emergent defibrillation (NOT synchronized)
- Correct electrolyte abnormalities (esp hypoK, hypoMg)
- Stop prolonged QT meds